Above Photo: A health-care worker vaccinates a woman with the Abdala jab in August. Yamil Lage / AFP via Getty.
Abstract
The purpose of this analytic essay is to contrast the COVID-19 responses in Cuba and the United States, and to understand the differences in outcomes between the 2 nations.
With fundamental differences in health systems structure and organization, as well as in political philosophy and culture, it is not surprising that there are major differences in outcomes. The more coordinated, comprehensive response to COVID-19 in Cuba has resulted in significantly better outcomes compared with the United States. Through July 15, 2021, the US cumulative case rate is more than 4 times higher than Cuba’s, while the death rate and excess death rate are both approximately 12 times higher in the United States. In addition to the large differences in cumulative case and death rates between United States and Cuba, the COVID-19 pandemic has unmasked serious underlying health inequities in the United States.
The vaccine rollout presents its own set of challenges for both countries, and future studies can examine the comparative successes to identify effective strategies for distribution and administration. (Am J Public Health. 2021;111(12):2186–2193.)
The purpose of this essay is to contrast the COVID-19 responses in Cuba and the United States. The 2 nations present widely varying examples of responding to the pandemic through governmental actions, surveillance and mitigation, testing, and public messaging, and the respective outcomes demonstrate the overall effectiveness of each country’s approach. Comparing the 2 will illuminate structural and organizational differences between the 2 health systems and how they have influenced COVID-19 outcomes.
Prepandemic Profiles
To better understand the influences and implications of each country’s actions during the pandemic, a general understanding of their health systems’ existing structure is required. The 1976 Cuban Constitution and the 1983 (Cuban) Public Health Law instituted the guiding principles for Cuba’s health system. Notable among these core values are “health care is a right, available to all equally and free of charge; health care is the responsibility of the state; [and] health care activities are integrated with economic and social development.”()
Although MINSAP (Ministerio de Salud Pública [Ministry of Public Health]) leads at the national level, it is community-level care that distinguishes the Cuban system. There are 11 128 consultorios (clinics) throughout the neighborhoods of Cuba, each staffed with a family doctor and nurse duo who often reside in the same community and are acutely familiar with the health status of the neighborhood and its residents. Family doctor and nurse teams are charged with health promotion, prevention, surveillance, rehabilitation, strengthening social cohesion, and other duties., The country’s nearly 500 polyclinics each oversee and support 20 to 40 of these consultorios., Municipal hospitals occupy the rung above polyclinics and provide more specialized care, and, above them, provincial tertiary care hospitals perform research. The Cuban health system was also designed without any delineation between public health and clinical care. Population health and medicine are inherently integrated at every level of the system, with sufficient allowance for local variance according to the unique needs of individuals and communities.
The US public health system is built on the principle of decentralization—that is, the role of the federal government in matters of public health is second to that of state and local governments. While medical care in the United States may be available to some through Medicaid (primarily for low-income individuals) or Medicare (for persons aged ≥ 65 years), for many people, health insurance is obtained through an employer and, therefore, dependent on employment. Across all forms of medical care, however, there are no guiding, agreed-upon values (e.g., affordability, accessibility, universality) to inform the systems that government or the private sector create, which has resulted in wide variability across the nation. Health coverage is not guaranteed, and 1 catastrophic health event could be the reason a person goes bankrupt. Thus, while the nation may be able to boast high-quality health care (for those who can access and afford it), the system remains rife with inequity and disparities.
In the sections that follow, the strengths and weaknesses of the 2 countries’ health systems will be exposed through an examination of the surveillance and identification of cases, mitigation strategies (including isolation and quarantine), testing, vaccine development, and outcomes, including the unmasking of health inequities in the United States.
Government Responses And Mitigation Strategies
Cuba’s response to COVID-19 began in January 2020, when the nation began surveilling arrivals at all ports of entry, and border and immigration officials received training on COVID-19 detection and response. In February, all personnel at hospitals and health care facilities were trained on COVID-19 prevention and treatment protocol. The first case of COVID-19 was detected in Cuba on March 11, 2020. Nine days later, Cuban President Díaz-Canel announced the first set of national measures aimed at combatting the spread of COVID-19. These earliest measures addressed both health and economic concerns—they included stay-at-home orders, bans on large gatherings, and many facilities being closed, as well as provisions for financial protection for certain high-risk groups and individuals, including small businesses or those hospitalized with COVID-19 and unable to work. In addition, outbound travel was limited to humanitarian efforts, and inbound travel was limited to Cuban residents who, upon arrival, were either hospitalized (if symptomatic) or ordered to quarantine at home (if asymptomatic).
This practice changed with improved testing capacity, and health staff began to administer COVID-19 diagnostic tests (reverse transcriptase‒polymerase chain reaction [RT-PCR]) to all arriving travelers in the airport, then hospitalizing the positive cases. Schools at all levels were closed indefinitely on March 23, police presence on the streets increased, and every law enforcement station was equipped with a district attorney to facilitate charges against any violators of COVID-19 restrictions. On April 1, the national mask mandate was instituted. An important characteristic of government response and mitigation strategies employed in Cuba has been “intersectoral participation,” with coordination across all high-level governmental units.
The US COVID-19 response also began in January 2020, when the Centers for Disease Control and Prevention (CDC) established a 2019-nCoV Incident Management Structure (January 7), and began screening for coronavirus at JFK International, San Francisco International, and Los Angeles International airports—the 3 US airports that receive the highest number of travelers from Wuhan, China. On January 21, the first case of COVID-19 was confirmed in Washington State, and, on January 31, the US Department of Health and Human Services secretary declared a US public health emergency. The US government announced its first set of national coronavirus mitigation measures on March 13, 2020. President Trump upgraded the previous declaration to classify the COVID-19 pandemic a national emergency, a designation that opened billions of federal dollars to be allocated to relief. A travel ban also went into effect, barring non-Americans who had been to any of 26 specific countries in the previous 2 weeks from entering the United States.
The federal government’s main approach to combatting COVID-19 was frequently said to be to “flatten the curve,” meaning to spread cases out over a longer period of time to avoid overwhelming the health system. As such, initial government actions occurred quickly and included strict isolation and shutdown measures in many parts of the country; however, the United States hastily moved to less stringent measures upon seeing only slight improvement. Implementation of stay-at-home orders, mask mandates, and other mitigation efforts were left to states’ discretion because of the decentralized nature of the United States’ public health system. A federal mask mandate would have likely received pushback on its constitutionality, but state-to-state variability made the use of masks much less effective as interstate travel was still permitted. On April 3, the CDC formally recommended the use of face coverings by the general public, and, by July 27, 31 states and the District of Columbia had issued statewide mask mandates. Like many other COVID-19‒related governmental efforts, the use of face masks became a politicized issue.
Surveillance And Case Detection
A unique feature of the Cuban response to COVID-19 has been its nationwide screening effort, which was enabled by the country’s strong primary health care system. Approximately 28 000 medical students volunteered to travel on foot in pairs to 80 to 100 homes and businesses every day, where they would ask how many individuals were present in the dwelling and if any had traveled, had respiratory symptoms, or had contact with a known COVID-19 case. Screening questionnaires were adapted to limit the likelihood of individuals hiding their symptoms and to promote early detection among high-risk populations.
The information was given to the consultorio family doctor, who passed it on to the coordinating polyclinic professor to be entered in a main database. The family doctor then provided follow up to individuals reporting respiratory symptoms. Existing data from the Continuous Assessment and Risk Evaluation—an annual assessment performed by family doctors to assess the general health of neighborhoods and residents—provided insight on higher-risk individuals who would require more attention. In addition to screening by medical students, these individuals with comorbidities also received regular follow up from family doctors. Symptomatic individuals and those with suspected contact with a known COVID-19 case were tested and, if positive, moved to an isolation center. Additional forms of ongoing surveillance include (1) monitoring all travelers arriving to Cuban ports, (2) testing suspected cases and the contacts of confirmed cases, and (3) postmortem testing on those who died with respiratory or diarrheal symptoms.
Screening and surveillance in the United States have been relatively disjointed. In the initial weeks of the pandemic, testing was limited to symptomatic individuals with a travel history to China; only later was testing made available for asymptomatic individuals both with and without known exposure to COVID-19. As testing became more widely available, CDC offered guidelines to include testing at-risk groups (e.g., workers with face-to-face interactions, residents of congregate settings, teachers, and first responders), and when the test positivity rate exceeds 10.1%, random screening should occur at least twice a week and all close contacts of confirmed cases should be tested. There was wide variety in how state and local governments and individual institutions and businesses implemented these recommendations.
Isolation, Contact Tracing, And Quarantining
In Cuba, every confirmed case of COVID-19 is hospitalized. After recovery, they are tested a second time and allowed to return home if negative. During the 15 days following their return home, those individuals are ordered to limit their movement out of the home and are provided follow-up from their local consultorio., All confirmed COVID-19 cases also undergo contract tracing. In the early months of the pandemic, those contacts identified were referred for obligatory quarantine in 1 of Cuba’s national isolation centers. As outcomes have improved, however, isolation requirements for contacts have eased, and suspected contacts are now permitted to complete a 14-day quarantine at home, monitored by their family doctor. Such broad, stringent isolation and contact-tracing efforts have been enabled by efficient horizontal and vertical data sharing. Robust communication about the status of cases and their contacts occurs throughout and across municipalities, provinces, and the nation.
In the United States, state and local isolation and quarantine orders for the general population have followed from CDC recommendations, which suggest that all individuals with a positive test result or who receive an exposure notification isolate at home for at least 14 days. The CDC later amended the guidance for asymptomatic individuals with suspected exposure, who are currently recommended a 10-day quarantine without testing or a 7-day quarantine if testing negative 5 days after exposure. These recommendations highlight the important consideration that testing and isolation orders go hand in hand: without being tested, asymptomatic, infected individuals are not made aware of the need to isolate.
It was estimated that between 100 000 and 300 000 tracers (numbers determined by population size) would be necessary to conduct effective contact tracing in the United States; however, with or without the human resources, widespread community transmission of COVID-19 has made any chance of large-scale contact tracing of every case very unlikely until the spread begins to slow. Some smaller-scale contact-tracing initiatives have been successful—for example those occurring on college campuses, often in tandem with local health departments. Although there have been instances of successful isolation orders and contact tracing, broad efforts have been greatly hindered in the United States by restrictions related to freedom, privacy, and civil liberties.
Testing
The tests used to diagnose infection with SARS-CoV-2—the virus that causes COVID-19—fall into 2 categories: nucleic acid amplification tests (NAATs) and antigen tests. NAATs are more sensitive, but the cost per test is high, and processing times are long. Antigen tests are more likely to deliver a false negative, but they are less expensive and provide quick results. In addition to these 2 diagnostic tests, there are antibody tests that can be used to detect evidence of past SARS-CoV-2 infection.
At the onset of the pandemic, Cuba was not equipped with the expensive, specialized infrastructure or trained personnel needed to implement mass RT-PCR testing (NAAT). To adapt and gradually build capacity, the nation prepared 7 diagnostic laboratories in regions across the country, and operated with the goal of a daily positivity rate below 10% of all tests. By October 2020, Cuba had reached a total of 13 diagnostic laboratories and, by April 2021, a total of 27 diagnostic laboratories, with at least 1 in every province. Although the process was slow-going in the early months, Cuban diagnostic facilities set the goal of performing high-volume testing to detect both symptomatic and asymptomatic cases.
Testing in the United States has been more complex than in Cuba’s experience. Like other COVID-19‒related efforts, it has largely been defined by disorganization by, and mixed messages from, the US federal government. The RT-PCR test developed by the CDC was the test used to detect the United States’ first case of COVID-19 in January 2020. Laboratories around the country were developing tests of their own at this same time; however, all diagnostic tests were required to obtain US Food and Drug Administration (FDA) Emergency Use Authorization (EUA) before use. The CDC’s test was the first to receive FDA approval, and shipments were sent to health departments in the early days of February. Only days later, they were found to be faulty. Other tests were available and ready to use, but the FDA’s EUA requirement placed a large bureaucratic barrier in the path, and it was not until February 29 that those tests (still without an EUA) were given the FDA’s green light for use.
The coordination did not improve from there. The United States suffered “inadequate and continued lack of testing” and “haphazard” administration of what tests were available (e.g., during the initial weeks of the outbreak, only symptomatic individuals with a travel history were tested, ignoring what was already known about community transmission in the United States). The failures in testing during the February‒April timeframe in particular played a large role in the inability to contain the pandemic.
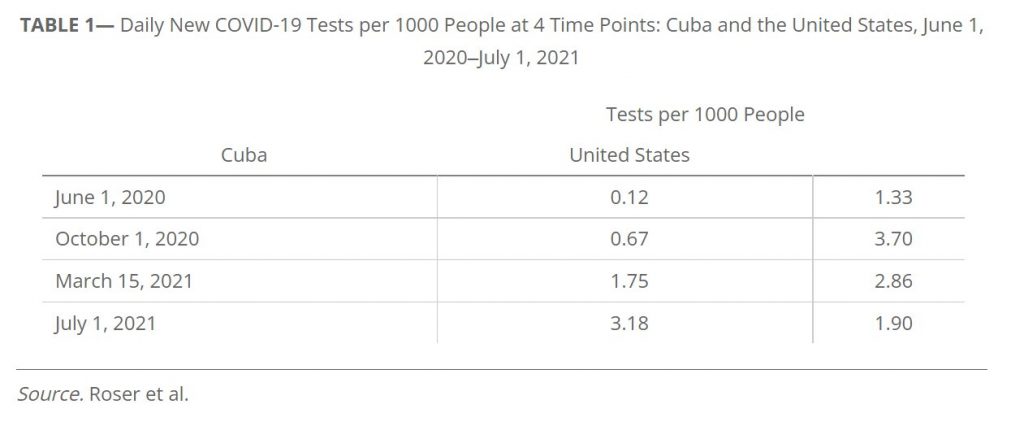
Table 1 displays the number of daily new COVID-19 tests performed per 1000 people in Cuba and the United States at 4 time points. Both countries demonstrated a steady increase in testing capacity over time; however, as Pérez Riverol confirms, testing capacity is better quantified as the number of COVID-19 tests performed per confirmed case. This metric considers the scope of the epidemic in a given area and better reflects whether the need for testing is being adequately met (Table 2).

Messaging
In the age of a proliferation of news and social media, health communication has become an essential step in combatting COVID-19. In Cuba, before COVID-19, state-owned television channels broadcast health education messages in place of commercials (as Americans know them). Strategic, informative communications related to COVID-19 began early in the pandemic, and health officials regularly provided “comprehensive stay-at-home messaging” that kept the public up to date and encouraged a collaborative spirit. These messages were provided during daily briefings broadcasted throughout the country as part of an “intense media campaign,” and they also included targeted information about people who were at most risk and the proper safety measures those individuals should take.
To combat misinformation, Cuba’s health network created the Web site Infecciones por coronavirus, which housed information from sources like the World Health Organization and Pan American Health Organization on the state of the pandemic and had a function allowing users to submit their questions to be answered by national experts. Juventud Técnica—Cuba’s only mass-circulation magazine focused on STEM (science, technology, engineering, and math) topics—initiated an effort to dismiss common rumors and debunk scientific misinformation. In addition to its fact-checking project, the publication also produced COVID-19‒related infographics and materials with information from government agencies like MINSAP.
COVID-19‒related messaging in the United States was characterized by conflict, inconsistency, and blatant misinformation. Many believe the Trump administration is largely to blame for the way scientific information was cast aside in favor of more self-serving messages that downplayed the severity of the US epidemic. Former President Trump publicly and repeatedly undermined the authority and expertise of the CDC and other health agencies. Under intense public scrutiny and facing criticism from the Trump administration, the CDC altered some of its previously published guidance despite objections from internal experts. This and other inconsistencies sowed doubt and distrust of the agency, as evidenced by the 16-point drop in the public’s trust in the CDC between April and September 2020. In response to the public’s growing uneasiness and concern about the safety of any vaccine put forward, 9 pharmaceutical companies released a statement in September 2020 affirming their loyalty to science over speed during the process of vaccine development.
Vaccine Development
Cuba’s January 2020 national COVID-19 control plan ordered the formation of an “innovation committee” to begin development of a vaccine. The nation boasts one of the world’s leading biotech industries, which comprises more than 30 research institutes and manufacturers and operates as the “state-owned conglomerate BioCubaFarma.” Because the industry is completely state-owned, -funded, and -operated, competition and the profit-driven actions of private companies have not been a factor in vaccine development. Although the country has had to navigate difficulty obtaining certain raw materials because of the US embargo, BioCubaFarma’s first vaccine candidate, SOBERANA01, was authorized by the Center for State Control of Medicines and Medical Devices to begin clinical trials in August 2020. As of March 2021, 2 (SOBERANA02 and Abdala) of Cuba’s 5 total vaccine candidates were in phase III clinical trials. Globally, a total of 21 other candidates had entered phase III trials by this time, and Cuba is the only Latin American country to have its own vaccine among that cohort. Abdala was shown to be 92.28% effective against symptomatic illness, and, in July 2021, it was authorized for emergency use. By July 14, 10.2% of the Cuban population was fully vaccinated with 3 doses, and another 41.6% had received either 1 or 2 doses. Cuba projects that the entire population will be vaccinated by the end of 2021. Cuban health authorities have been vocal about their intention to distribute vaccine doses internationally, especially to countries within the Global South, as domestic rollout continutes.
Multiple private companies have been involved in the process of developing a vaccine for use in the United States. The public‒private partnership between those companies and the US government was first publicly announced by the Trump administration in May 2020. The effort was named Operation Warp Speed (OWS), and its initial goal was to have “substantial quantities” of a safe COVID-19 vaccine by January 2021. Nearly $10 billion was allocated by Congress to OWS to fund efforts in development, manufacturing, and distribution. By October 2020, OWS had announced partnerships with 6 companies: Moderna, Pfizer‒BioNTech, AstraZeneca, Johnson & Johnson, Novavax, and Sanofi/GSK. In November 2020, both Pfizer and Moderna released promising results from phase III clinical trials. Days later, Pfizer became the first company to submit its vaccine candidate to the FDA for EUA, and in mid-December, the FDA granted EUAs for both the Pfizer and Moderna vaccines. Moving the vaccine from initial development to injecting it into people’s arms in less than 1 year was a monumental achievement. In February 2021, the 1-dose Johnson & Johnson vaccine also received EUA from the FDA.
As of July 15, 2021, 48% of the US population was fully vaccinated against COVID-19, with another 7.4% partly vaccinated. The United States has not been without its fair share of distribution challenges. In the first few weeks of vaccine rollout, while CDC had provided guidance for prioritization, implementation at the state level was inconsistent and did not necessarily abide by CDC’s recommendations. During the first several weeks of vaccine rollout, more vaccine doses were delivered (per capita) to Whites compared with people of color. The United States has also had major challenges in overcoming vaccine disinformation and vaccine hesitancy.
Cases, Deaths, And Inequities
The COVID-19 pandemic has resulted in astoundingly different outcomes between the United States and Cuba, as shown in Table 3, which displays the cumulative numbers and rates of cases and deaths of both countries through July 15, 2021: the US cumulative case rate is more than 4 times higher than Cuba’s, while the death rate and excess death rate are both approximately 12 times higher in the United States.
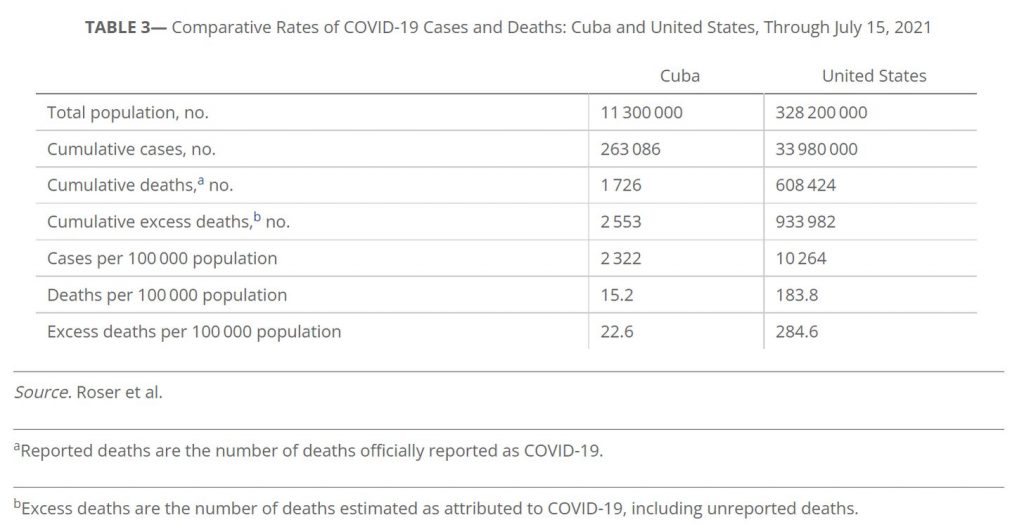
In addition to the large differences in cumulative case and death rates between United States and Cuba, the COVID-19 pandemic has unmasked underlying health inequities in the United States that, while understood in the public health community, were previously not in the public conscience. The immense contrast between COVID-19 outcomes in the United States and in Cuba and their correlation with certain organizational mechanisms of their health systems cannot be denied. In Cuba, mortality rates from COVID-19 and the number of confirmed cases has been balanced equally across socioeconomic strata. Provincial diagnostic facilities and neighborhood consultorios have meant that testing and therapeutics are equally accessible for residents of both urban and rural areas. By contrast, racial/ethnic minority groups in the United States have COVID-19 mortality rates twice as high as that of White Americans. Also, low-income Americans have borne the brunt of the financial impacts of COVID-19 (e.g., unemployment, food insecurity) in addition to worse health outcomes. These disparities arise from structural shortcomings like inefficient health coverage systems, inadequate health care infrastructure, and misuse of existing resources. Inequities have also been exposed in the areas of testing and vaccinations.
Conclusion
Although Cuba and the United States differ from one another in numerous ways, their respective experiences—especially outcomes—signal clear failures in the United States. The more coordinated, comprehensive response to COVID-19 in Cuba has resulted in significantly better outcomes compared with the United States. Much of this difference can be attributed to the structure of the countries’ health systems. In Cuba, MINSAP has taken charge at every level: from provision of health services to preserving the system’s universality and affordability even in the face of a global health crisis. In the United States, a decentralized structure has allowed for the diffusion of authority and accountability across multiple federal and state agencies, and no clear leader has emerged. Thus, it can be argued that the organization of the Cuban and US health systems was a primary determinant of their pandemic response because, respectively, they produced either consistency and clear direction, or disorganization and conflicting guidance.
In addition to structural differences, Cuba and the United States differ in their general trust of concentrated power. Pandemic response greatly relies on health protection measures and decisive leadership, which have been perceived as infringement on individual liberty by many Americans. In Cuba, the adoption of strict control measures and adherence to governmental guidance by most residents undoubtedly facilitated the successful COVID-19 response. It is questionable whether comparable actions would have been widely accepted by residents of the United States, but without a well-integrated health system, it is inconceivable that they could have been properly implemented—regardless of public opinion.
At the time of writing, the COVID-19 pandemic continues to evolve. In the United States, after a post-Thanksgiving (2020) to New Years’ surge (2021), the 7-day rolling averages of new cases and deaths steadily trended downward through late March 2021, followed by another rise. By May 2021, numbers trended down, and then again creeped upward in the early days of July 2021. After months of relatively low case rates, Cuba experienced a surge in cases and deaths between January and March 2021, followed by a plateauing. In mid-June 2021, Cuba again saw a surge to an all-time high of nearly 7000 new cases in 1 day in mid-July. The increase is attributed to new, more contagious variants, the public’s decreased risk perception because of months of low cases and the introduction of vaccines, and the ineffectiveness of renewed efforts to limit transmission through restricting movement of individuals. Between February and June 2021, the reproduction rate in Cuba and the United States remained at and below 1.0, respectively. By June 15, the reproduction rate began to rise in both countries, reaching 1.5 on July 10, 2021. Neither country has moved beyond the pandemic, and further research may examine potential differences in the easing or tightening of COVID-19‒related restrictions in Cuba and the United States and the subsequent effects. The vaccine rollout presents its own set of challenges for both countries, and future studies can examine the comparative successes to identify effective strategies for distribution and administration.

